By: Ann Avery, MD, Infectious Disease Physician at MetroHealth Medical Center
Being HIV-positive doesn’t mean you can’t have sex. Once you know you have HIV, you know you don’t want to give it to somebody else. Yes, HIV is usually transmitted through sexual activity, so it’s tempting to think your sex life is over once you’ve been diagnosed. However, that is not even remotely true.
As someone living with HIV, you just have to have sexy time in a way that keeps that pesky HIV virus away from the pathways into your partner’s body, such as the mucous membranes of the anus and the vagina.
This should be done regardless of your partner’s HIV status, as no two strains of HIV are the same. It’s just a matter of the two of you having an honest and straightforward discussion and finding ways to be intimate that don’t risk transmitting the virus. There is a buffet of options at your disposal, find the ones that work for you and your partner and have some safer, smarter fun!

Condoms and STI Risk
Condoms are a great option. While they are not perfect, they are extremely reliable and come in a variety of flavors, colors, shapes, and some even glow in the dark! Yes, some people don't like sex with a condom, but they still represent one of the best ways to prevent HIV transmission.
It’s also important to note that, unlike other prevention tools, Condoms prevent the spread of other sexually transmitted infections (STIs) like syphilis, gonorrhea and herpes too. Anyone living with HIV wants to avoid contracting additional STIs — there are just too many potential complications.
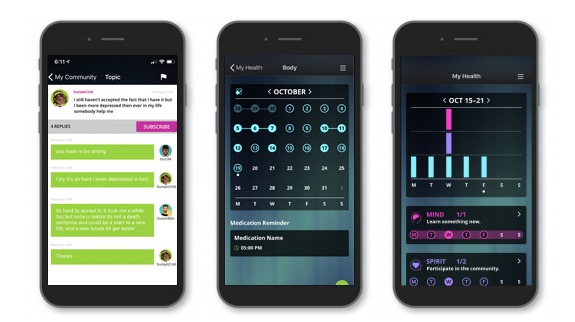
Come join our private, stigma-free, supportive community.
Health management tools with medication & appointment reminders.
Social networking in a community conversation & private chats.
Is There a Medicine That Prevents HIV?
Yes, yes there is. PrEP (Pre-Exposure Prophylaxis) is the once daily dose of the anti-HIV medicine, Truvada, to prevent HIV infection in someone who is HIV negative (It is not for someone already living with HIV). When taken as prescribed, PrEP is up to 99% effective at preventing HIV! A HIV-negative partner can take PrEP once a day, seven days a week, to defend their body from becoming HIV infected should they accidentally be exposed. It takes roughly 1 week of daily use to be optimally protected during anal sex and up to 3 weeks for optimal protection during vaginal sex. It is important to note, PrEP does not protect against any other STI’s. It is only effective at preventing HIV infection so the use of condoms is still encouraged. This is especially true when the partner’s STI status is unknown or in question.
Another option, called PEP (Post-Exposure Prophylaxis), allows an HIV-negative person to start taking HIV meds within 72 hours of their potential exposure to HIV to reduce their chances of becoming infected. Once they have started their regimen, the individual will continue to take the medicine as prescribed for about a month. While this is not ideal, it is an option in case a situation should arise where potential HIV transmission has occurred.
Achieving an undetectable viral load and what that means for HIV prevention
For individuals living with HIV, there is no greater feeling than to hear you have an undetectable viral load. Being undetectable means the anti-retroviral therapy (ART) is working and has stopped HIV from replicating, thus lowering the amount of HIV in the bloodstream and allowing the immune system to bounce back to a normal level. It’s a fist pump and high five worthy moment for sure, but it doesn’t end there. An undetectable viral load is also good strategy for HIV prevention. Being undetectable significantly reduces the chance of HIV transmission during sex. How cool is that?!
These are all attractive options. Keep educating yourself and choose the option(s) that are right for you and your partner(s).

Living with HIV When Both Partners are Positive
People with HIV sometimes gravitate into relationships with other people who living with the virus.
Having an HIV-positive partner can take a lot of the angst out of a relationship because you’re both going through the same thing and can be a great support to one another.
One thing to keep in mind, though, is that you still want to avoid the possibility of passing along other STIs. For another, the two of you are likely infected with different strains of the virus, and if you’re not undetectable, you could potentially expose one another to the risk of secondary infection that can complicate your treatment.
The main things to remember when it comes to having sex with HIV are to understand the risks, be adherent to your medicine, know what safer sex tools are available to you and your partner(s), and use them. In the realm of sex, relationships, and intimacy, the responsibility lies with you to make the best decisions to protect your health and the health of your partners.
Positive Peers is made possible through a U.S. Department of Health and Human Services Health Resources and Services Administration, HIV/AIDS Bureau Special Projects of National Significance (SPNS) Grant to The MetroHealth System. Click here for more information about the SPNS grant initiative.
Positive Peers is a private app for young people living with HIV. Learn how you can earn rewards for your participation.