By: Ann K. Avery, MD, Infectious Disease Physician at MetroHealth Medical Center
These are some of the most common terms about HIV, AIDS, the immune system, HIV treatments, HIV testing and HIV prevention.
HIV Basic Terms
 HIV
HIV
Human Immunodeficiency Virus. A virus that attacks the immune system and makes it difficult to fight off diseases. Medications to fight HIV can prevent the development of AIDS.
 AIDS
AIDS
Acquired Immune Deficiency Syndrome. AIDS happens after HIV has damaged the immune system, usually over the course of several years.
 Poz
Poz
Shorthand for somebody who is HIV positive (often reads as “poz people” or “a poz person.”) Also the name of a popular website and magazine for HIV-positive people: www.poz.com.
 Seroconversion
Seroconversion
The point when a person’s bloodstream becomes infected with HIV.
Immune System Terms
 CD4
CD4
A special kind of white blood cell that sounds the alarm to the immune system to send antibodies to attack germs, bacteria, fungi, and viruses (like HIV) in the bloodstream. HIV destroys CD4 cells, but only after using them to make copies of itself in the bloodstream.
 CD4 count
CD4 count
This is also called “t-cell count” - An estimate of how many CD4 cells are in your bloodstream. A normal CD4 count is about 500-1500. Doctors usually diagnose AIDS if the CD4 count falls below 200.
 Opportunistic Infections
Opportunistic Infections
Infections that attack a weakened immune system. Healthy bodies usually fight off these infections. Opportunistic infections mostly happen when the CD4 count has fallen below 200, and are avoidable if HIV is treated early and medication is adhered to, keeping CD4 count high and the immune system healthy.
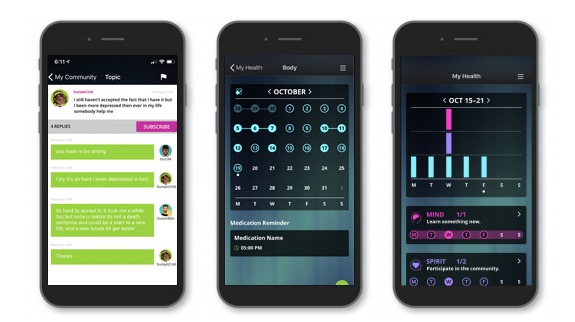
Come join our private, stigma-free, supportive community.
Health management tools with medication & appointment reminders.
Social networking in a community conversation & private chats.
HIV Treatment Terms
 Adherence
Adherence
Sticking to a drug regimen. Anti-retroviral drugs must be taken every day for life.
 ART or ARVs
ART or ARVs
Anti-Retroviral Therapy or Anti-RetroVirals. Medicine to treat HIV (which doctors call a retrovirus). It takes at least 3 different ARVs to treat HIV, but there are many ARVs that have been combined into just one pill, once-a-day.
 Prophylaxis
Prophylaxis
Action that prevents disease or offers protection from disease.
 PreP
PreP
Pre-Exposure Prophylaxis. HIV-negative people can take this drug therapy to reduce their risk of contracting HIV. It is recommended for
- sexually active MSMs (men who have sex with men) who are at risk of HIV infection
- sexually active heterosexual men and women who are at risk of HIV infection
- injection drug users who are at risk of HIV infection
- sexually active men and women whose partners are HIV-positive
 PEP
PEP
Post-Exposure Prophylaxis. Taking these drugs within 72 hours of exposure can dramatically reduce the risk of getting an HIV infection.
HIV Testing Terms
 False positive
False positive
Inaccurate results of an HIV test. A false positive happens when the test mistakenly says you are HIV positive. This is why it takes 2 different types of HIV tests (and occasionally a third) to confirm an HIV infection.
 Viral load
Viral load
A test that measures how much HIV is in your bloodstream. Viral loads are extremely high in the first few weeks after exposure (like millions of copies of virus). ART can reduce viral load until it is undetectable (less than 20 copies) (even if undetectable, HIV will still be in the bloodstream. It’ll just be too rare to show up in tests).
HIV Prevention Terms
 Safer sex
Safer sex
Using condoms, other barriers such as female condoms and dental dams, and following other common guidelines to prevent bodily fluids from coming into contact and causing an HIV or other sexually transmitted infection.
 Risk factors
Risk factors
Anything that increases the likelihood of transmission of HIV, including risky behaviors and belonging to certain groups where HIV infections are more common.
 High-risk activities
High-risk activities
Specific acts that have a proven connection with transmitting HIV. Unprotected receptive anal sex and sharing needles for drug use are the most common high-risk activities. It’s also possible for mothers to pass HIV to their babies in breast milk, so moms living with HIV should not breast feed.
Positive Peers is made possible through a U.S. Department of Health and Human Services Health Resources and Services Administration, HIV/AIDS Bureau Special Projects of National Significance (SPNS) Grant to The MetroHealth System. Click here for more information about the SPNS grant initiative.
Positive Peers is a private app for young people living with HIV. Learn how you can earn rewards for your participation.