By: Ann K. Avery, MD, Infectious Disease Physician at MetroHealth Medical Center
If you think you might be at risk of becoming infected with HIV — but you’re not infected already — you really need to know about PrEP.
PrEP is the once-daily use of the medicine Truvada by an HIV-negative individual to significantly reduce their chances of becoming infected by HIV. When taken as prescribed, PrEP is proven to be up to 99% effective at preventing HIV infection!
The most obvious candidate for PrEP is an HIV-negative person with an HIV-positive partner.
Other candidates for PrEP include:
- Men who have had unprotected anal sex with other men in the past six months, or who have contracted a sexually transmitted disease in the past.
- Anybody who is unsure of the drug or sex habits and histories of their current partners, but has a strong reason to suspect their partner could be living with or become exposed to HIV.
- Injection drug users who share needles
- Anyone with multiple sex and/or drug-sharing partners, especially if the partners’ HIV statuses are unknown
- Individuals who exchange sex for money, shelter, food, and/or other services.
If you’re in any of these groups, you should talk to your doctor about PrEP right away. If taken correctly, PrEP can reduce your chance of getting infected by up to 99%, when used correctly.
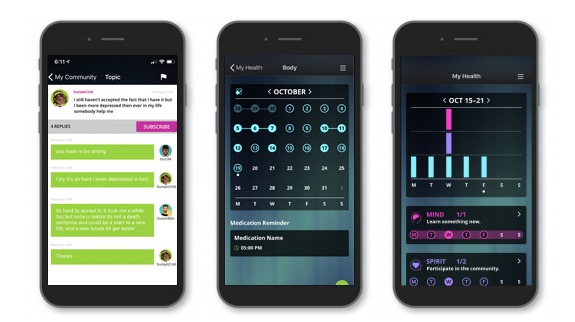
Come join our private, stigma-free, supportive community.
Health management tools with medication & appointment reminders.
Social networking in a community conversation & private chats.
How PrEP works
PrEP is short for “Pre-Exposure Prophylaxis.” Pre-exposure means you take it before you’ve been exposed to HIV. If you already have HIV, you’ll need to take different meds.
If you’ve ever heard a condom called a “prophylactic,” you already have an idea of how PrEP works. To put it bluntly, PrEP is like a condom for your immune system.
It’s not a latex tube like the ones you use for smarter, safer sex. It’s a chemical barrier scientists designed for one specific job: protecting certain immune system cells against attacks by HIV. It does not protect someone from any other STI, only HIV.
The PrEP effect
HIV hijacks CD4 t-cells that the immune system needs to fight off infections. Once HIV takes over a CD4 cell, it makes a bunch of copies of itself and then kills off the CD4 cell. After that, all those copies of HIV go looking for more CD4 cells to hijack and kill.
If the CD4 cells have no protection from HIV, the virus can make billions of copies of itself and cause an infection.
PrEP uses a pair of chemicals that prevent HIV from attaching itself to CD4 cells. It works much like a suit of armor to protect those lovely CD4 cells! If HIV can’t get into the CD4 cells, it can’t spread, and it can’t turn into an infection.
What PrEP isn’t

Now that you know what PrEP is, you need to understand what it isn’t.
- It’s not a cure for HIV.
- It’s not a vaccine for HIV.
- It’s not a replacement for condoms during sex.
- It’s not for people who already have HIV.
- It’s not a free pass to engage in risky behaviors.
Important considerations for PrEP
- PrEP should be taken once a day, every day. Its effectiveness plunges if you don’t take it regularly as directed.
- PrEP needs to build up in your body for at least a week before it becomes effective for oral and anal sex and at least three weeks for vaginal sex
- You have to be tested for HIV before you start PrEP, and you need to see your doctor every three months as long as you’re taking it for a few screenings and your refills
- The drug used for PrEP is called Truvada. If you don’t have insurance, you will almost certainly need help paying for it and that help is available. If you have insurance with prescription drug coverage, it will very likely cover it but there are other forms of assistance available to help supplement that coverage if you qualify.
PrEP isn’t a cure-all. After all, it’s not even a cure. If you might be at risk for HIV, PrEP is an important and exciting prevention tool that you can add to your safer sex tool belt.
Talk to your doctor and ask if PrEP is a good option for you.
Positive Peers is made possible through a U.S. Department of Health and Human Services Health Resources and Services Administration, HIV/AIDS Bureau Special Projects of National Significance (SPNS) Grant to The MetroHealth System. Click here for more information about the SPNS grant initiative.
Positive Peers is a private app for young people living with HIV. Learn how you can earn rewards for your participation.