People who think HIV is a disease of gay men probably haven’t seen the facts on how many straight women are infected.
More than 20 women become infected with HIV every day in the United States. That’s about one-fifth of all the new HIV cases reported, according to 2014 data from the federal Centers for Disease Control and Prevention.

By: Ann K. Avery, MD, Infectious Disease Physician at MetroHealth Medical Center
Women have it worse worldwide — they account for about 60 percent of all new HIV diagnoses for people between ages 15 and 24. Sub-Saharan Africa has eight out 10 of all young women infected with the disease, according to the United Nations. Most women contract HIV through heterosexual contact or injection drug use.
HIV is not picky about the ages of the women it infects. In recent years a number of women in the in their 40s, 50s and older have become infected.
Turns out safer sex is the way to go at every age.
How Women Contract HIV
The tissues of the vagina are soft and porous, making it easy for HIV to pass from semen (cum) into the bloodstream. Any woman who has unprotected sex with an HIV-positive man has the potential to get infected.

A straight woman with an HIV-positive male partner can easily contract the virus from him. It’s much harder for a woman to pass along HIV to a man via vaginal sex because only a small section of the penis has tissues that are vulnerable to HIV.
Women who use injected drugs and share needles face the same risks as men.
Key HIV Issues for Women
Once HIV gets into the bloodstream, it attacks the immune systems of men and women pretty much the same way.
Women can take anti-retroviral drugs to fight back against HIV and lead normal lives. Some HIV drugs have side effects specific to women, so it might take a while to settle on the best regimen.
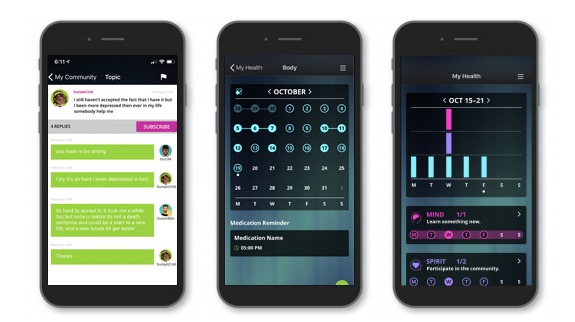
Come join our private, stigma-free, supportive community.
Health management tools with medication & appointment reminders.
Social networking in a community conversation & private chats.
Women who test positive while they’re pregnant need to be on anti-retrovirals (ideally the entire pregnancy, but at least from the second trimester on) to reduce their viral load, hopefully to undetectable. The lower the viral load at the time of labor and delivery, the less chance they have of passing HIV along to their baby. In fact, with anti-retroviral treatment during pregnancy, an IV drip of medicine during labor and delivery, and 6 weeks of medicine for the baby after birth, mother-to-child HIV transmission risk is as little as just 1%! (versus around 30% if mom doesn’t receive treatment and this protocol isn’t followed).
Because HIV attacks the immune system, women have to be on the watch against certain female-specific maladies. Recurrent yeast infections, for instance, can be a serious issue for HIV-positive women.
All women who are living with HIV need to have an in-depth talk with their HIV doctors about all the potential issues that are specific to female physiology.
Knowing All the facts on Women and HIV
Women should think about the best ways to protect themselves from HIV infection. That means sex with a condom or other barrier method (eg, dental dam, female condom) every time if you have any reason to suspect your partner has been exposed to the virus. Another option is to talk to your doctor about PrEP, a prescription medicine taken once-a-day to prevent HIV infection.
Once you get on anti-retroviral meds, certain tests will reveal how well the drugs are doing at decreasing your viral load (viral load test) and strengthening your immune system (CD4 count).
In the U.S., HIV-positive diagnoses of women plunged 40 percent between 2005 and 2014, according to government data.
That’s welcome news — but the numbers can always go lower. Getting tested, taking anti-retroviral meds if you’re living with HIV, and following safer-sex practices are still the best ways to make that happen.

Positive Peers is made possible through a U.S. Department of Health and Human Services Health Resources and Services Administration, HIV/AIDS Bureau Special Projects of National Significance (SPNS) Grant to The MetroHealth System. Click here for more information about the SPNS grant initiative.
Positive Peers is a private app for young people living with HIV. Learn how you can earn rewards for your participation.