By: Ann K. Avery, MD, Infectious Disease Physician at MetroHealth Medical Center
Hepatitis is another h-word that if you’re already living with HIV, you may not want to hear anything about it. But there are some good reasons why it’s important to know how the virus works and how you can prevent yourself from getting it.
Hepatitis can make it trickier to fight HIV and stay healthy, and viral hepatitis causes more deaths in the U.S. than HIV, according to the Centers for Disease Control and Prevention. (In 2014, viral hepatitis claimed 8,081 lives vs. 6,721 for HIV.)
The main challenge of HIV and hepatitis is managing both at the same time — what doctors call a “co-infection.” The good news is if you’re already in treatment for HIV, you know what you have to do. Hepatitis just adds a few items to your to-do list.
Let’s take a deep dive into the facts about HIV and hepatitis.
What is hepatitis?
Hepatitis means inflammation of the liver. The liver doesn't work well when it’s inflamed, which is a big deal because the liver cleans toxins out of the blood and helps the body process nutrients and medications.
As we’ve said a dozen times on Positive Peers, staying healthy when you’re living with HIV means taking your meds every day and eating a healthy diet. Your liver plays a big part in making that happen, so it needs all the help that it can get to work properly and keep you healthy.

Can hepatitis be treated or cured?
It depends on which kind we’re talking about. Medicines can treat or cure specific varieties of hepatitis, and vaccinations can prevent other varieties.
Before talking about treatments and cures, the most important first step with hepatitis is getting tested to see if you have it. Tests can figure out exactly which kind you have. And if you test negative, your doctor may suggest that you get vaccinated.
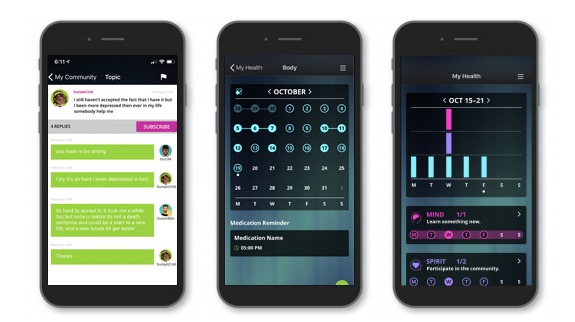
Come join our private, stigma-free, supportive community.
Health management tools with medication & appointment reminders.
Social networking in a community conversation & private chats.
Why is viral hepatitis so serious?
Viral hepatitis and HIV usually go together because people can get the viruses for the same reasons. This normally is through injecting drugs with used needles or having unprotected sex with someone who is living with the virus. But there are still other ways you can get hepatitis, which we’ll go into later in this blog.
About one-third of the people living with HIV also have viral hepatitis. If you’re sitting in a room with 10 people living with HIV, there’s a fair chance that three of them have viral hepatitis. And just like HIV, the first step to treatment is getting tested so you know if you have it. Then, you can work with your doctors to fight it.

How can I tell if I have hepatitis?
- Symptoms of hepatitis include:
- Jaundice (yellowing of the skin and the whites of the eyes)
- Fatigue
- Nausea/vomiting
- Poor appetite
- Dark urine
- Feeling dazed or disoriented
Symptoms vary depending on the person and which variety of hepatitis they have. But sometimes, there are no symptoms at all! Testing helps your doctor to determine if you have hepatitis, which kind, and what the best treatment is.

What are the three most common varieties of viral hepatitis?
Scientists use letters of the alphabet to identify different kinds of hepatitis. We use “hep” and three-letter titles to divide them up. The transmission, treatment, and prevention of viral hepatitis vary quite a bit from one variety to the next, so it helps to look at them separately:
Hep A (HAV)
Most people recover completely from hepatitis A with no liver damage. It often passes from the hands of people who are infected into the foods and drinks they prepare for other people.
- Transmission:
- Sexual contact
- Consuming food or drinks prepared by someone with the virus
- This is spread through fecal matter — tiny bits of bacteria on someone’s hands from changing a diaper, touching injection-drug works, or going to the bathroom without washing their hands.
- Treatment:
- HAV often is removed from the body naturally, meaning no medications are usually needed.
- Prevention:
- Vaccination
- Sanitation
- Protected sex
- Avoiding injected drugs
Hep B (HBV)
Some people get over the hepatitis B virus naturally, though some develop long-lasting infections. It’s more likely to be spread by sexual contact than other means.
- Transmission:
- Infected blood, semen (cum), and other bodily fluids
- Contaminated needles
- Pregnant mother to her unborn child
- Treatment:
- Rest and recuperation for short-term infections that can go away on their own
- Anti-viral medications for long-term infections that don’t go away
- Liver transplant for life-threatening liver damage
- Prevention:
- Vaccination (mothers can be vaccinated during pregnancy to prevent infecting an unborn child)
- Condoms and safer sex
- Avoiding alcohol and injected drugs
- Using only new needles and works
Hep C (HCV)
Hepatitis C was long considered incurable, but we now have medicines that can cure it in most people. Hep C often hides in the blood for decades. If untreated, it may lead to liver cancer or other serious liver diseases.
- Transmission:
- Contact with the blood of a person with the virus
- Contaminated needles
- Unprotected sex
- Needle sticks
- Treatment:
- Anti-viral medications
- No vaccine available
- Prevention:
- Using only new needles and works
- Condoms and other safer-sex practices
Living with co-infections
Hepatitis can complicate your HIV treatment, but it’s totally possible to treat both. You may already be living with HIV and hepatitis and not know it, so getting tested is your best bet to make sure you can fight the virus before it causes more damage.
The liver may not get the same credit the heart and the brain get for keeping you healthy and functioning, but it’s just as important to have your other organs working to their top potential. By protecting your liver, you let your meds go about their business of keeping you healthy.
Related Blogs: